Exploration of Immunotherapy: Scientists Discover Methods to Forecast Results
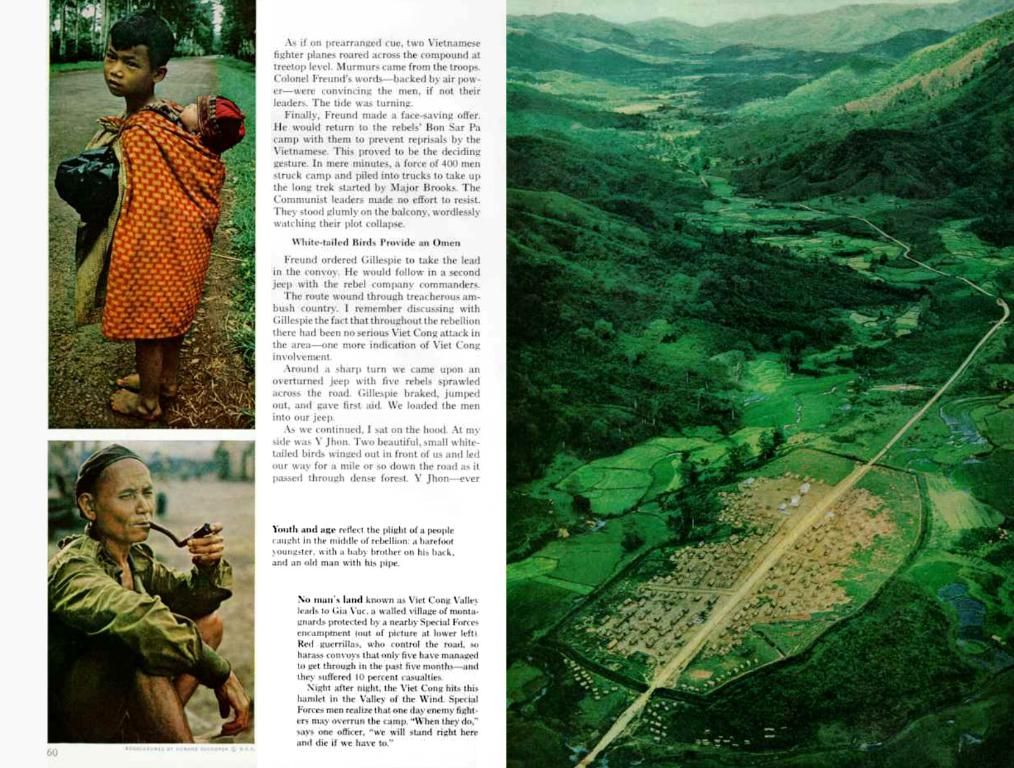
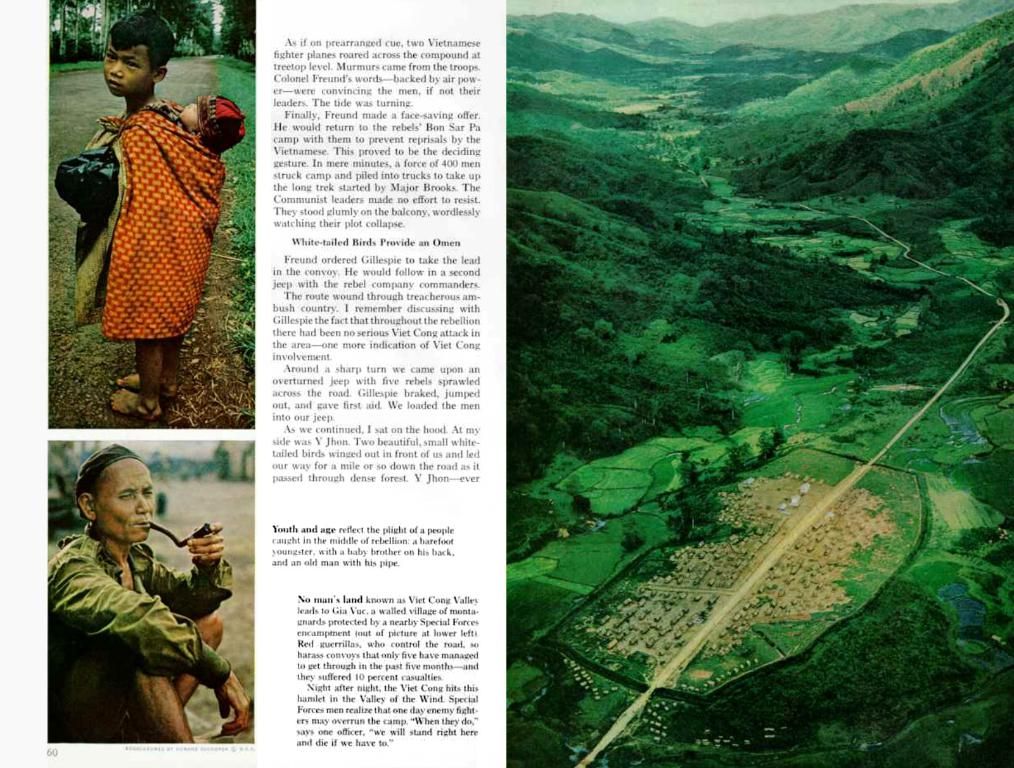
immunotherapy, a cutting-edge cancer treatment utilizing the body's immune system, isn't a one-size-fits-all solution. Not every individual with cancer, nor every type of cancer, responds positively to it. To solve this conundrum, researchers from Johns Hopkins University in Maryland have identified a specific group of mutations within a cancer tumor – the so-called 'persistent mutations' – that could potentially clue healthcare providers into the likelihood of a successful immunotherapy response.
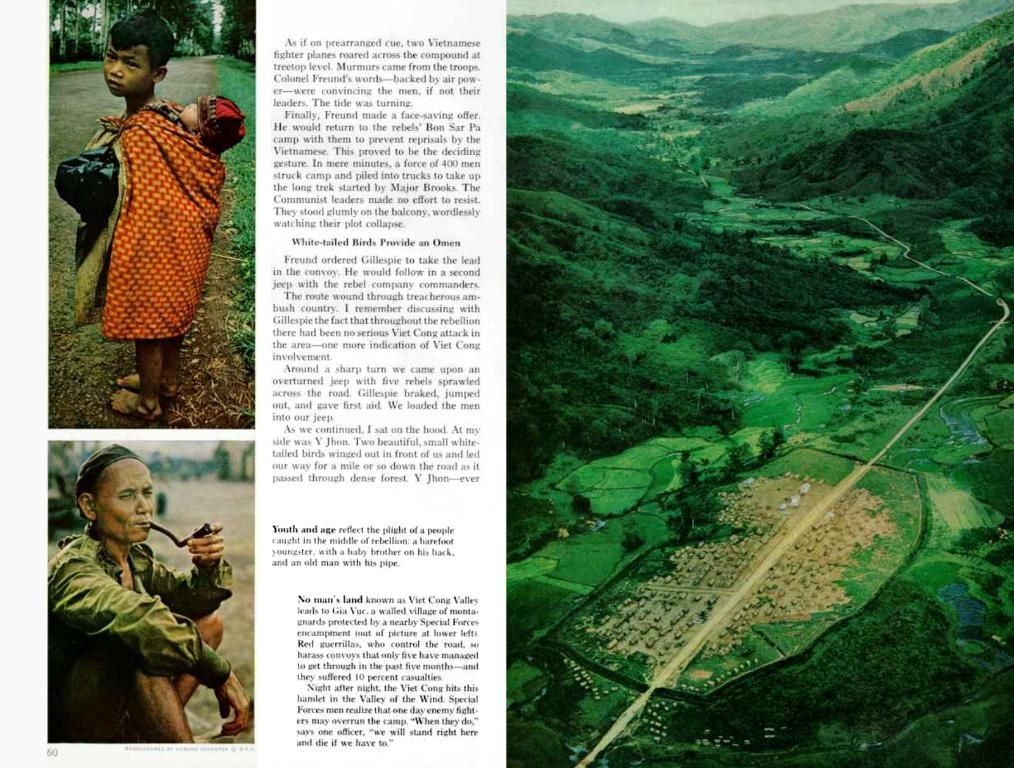
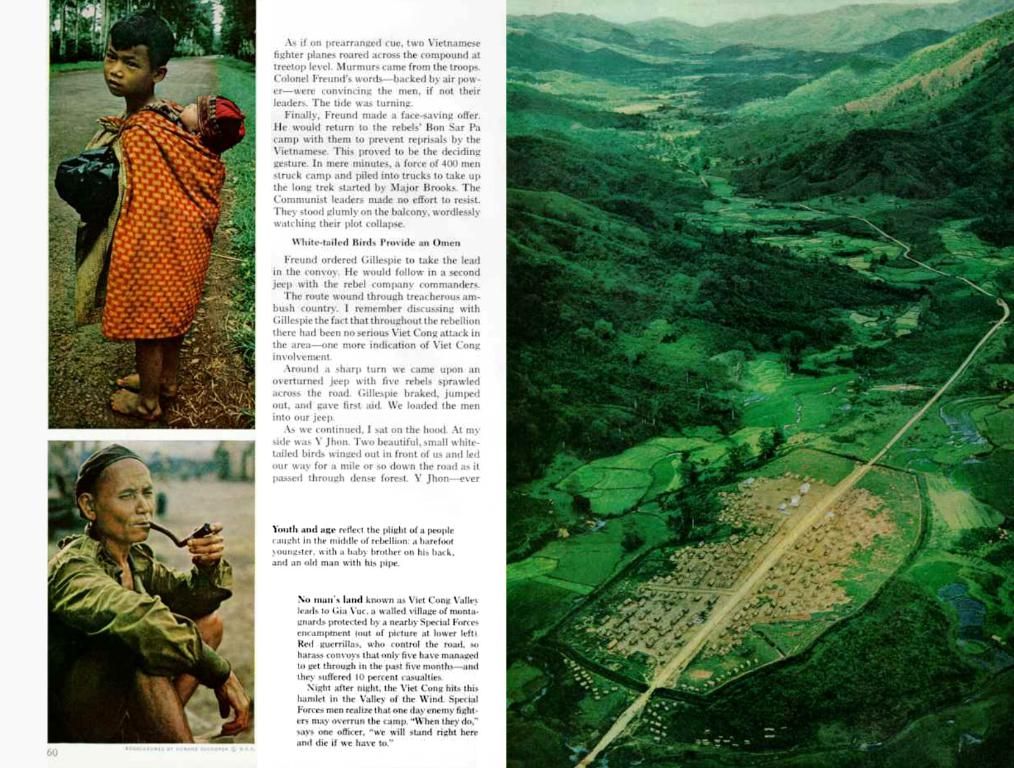
In essence, these persistent mutations ensure that cancer cells remain easily identifiable by the immune system, making it easier for the body to recognize and eliminate the malignant cells. This discovery could revolutionize cancer treatment selection and provide a clearer picture of the potential outcomes from immunotherapy.
The researchers published their findings in the journal Nature Medicine. So, what exactly are these persistent mutations, and how do they affect cancer treatment outcomes?
Immunotherapy leverages the power of the immune system to attack and eradicate cancer cells. Typically, cancer cells undergo mutations allowing them to evade the immune system. Immunotherapy seeks to overcome this resistance by strengthening the body's immune response.
Currently, immunotherapy shows promise for breast cancer, melanoma, leukemia, and non-small cell lung cancer. Researchers are also stretching its potential towards fighting other types of cancer, like prostate, brain, and ovarian cancer.
At present, doctors estimate a cancer tumor's likelihood of responding to immunotherapy based on the total number of mutations in the tumor, known as the tumor mutation burden (TMB). Dr. Valsamo Anagnostou, a senior author of the study and associate professor of oncology at Johns Hopkins, explains, "Tumor mutation burden is the number of changes in the genetic material and particularly in the DNA sequence of cancer cells, known as mutations."
In this study, Anagnostou and her team delved deeper into the mutations within the TMB and identified a specific subset – the 'persistent mutations' – that persist even as cancer evolves. This trait allows the cancer tumor to stay visible to the immune system, which in turn improves the response to immunotherapy.
Anagnostou adds, "Persistent mutations are always there in cancer cells and these mutations may render the cancer cells continuously visible to the immune system, eliciting an immune response. This response is augmented in the context of immune checkpoint blockade and the immune system continues to eliminate cancer cells harboring these persistent mutations over time."
In short, the number of persistent mutations provides a more accurate assessment of a tumor's receptiveness to immunotherapy than the TMB alone. This insight could help doctors more precisely select patients for immunotherapy and improve the prediction of treatment outcomes.
Dr. Kim Margolin, a medical oncologist and medical director of the Saint John's Cancer Institute Melanoma Program at Providence Saint John's Health Center in California, noted, "It was refreshing to see this highly-respective collaborative group has gone beyond the simple concept of tumor mutation burden, loss of mutation-containing sequences, and defined persistent mutations in a new light."
In the future, it's likely that high-throughput, next-generation sequencing techniques will be employed to study patients' mutational spectrum, categorizing them based on their likelihood of responding to immunotherapy. This promises a more personalized approach to cancer treatment, tailored to an individual's unique genetic profile.
As our understanding of cancer and immunotherapy evolves, we step ever closer to creating a cancer treatment landscape tailored to the individual, harnessing the power and resilience of the body's own immune system.
- The persistent mutations, a specific subset of mutations within a cancer tumor, could potentially provide healthcare providers with a clearer picture of the likelihood of a successful immunotherapy response.
- These persistent mutations make cancer cells easily identifiable by the immune system, enhancing the body's ability to recognize and eliminate malignant cells.
- The identification of persistent mutations has the potential to revolutionize cancer treatment selection, as they provide a more accurate assessment of a tumor's receptiveness to immunotherapy than the tumor mutation burden (TMB) alone.
- By employing high-throughput, next-generation sequencing techniques to study patients' mutational spectrum, researchers aim to categorize patients based on their likelihood of responding to immunotherapy, promising a more personalized approach to cancer treatment.