Personalized Care Approach Focused on Lifestyle Factors May Decrease Risk of Atrial Fibrillation
Atrial fibrillation, often just called "AFib," is a heart issue characterized by an unpredictable beating of the upper heart chamber. This can potentially cause blood clots and increase the risk of stroke.
Beyond well-known factors related to cardiovascular health, like physical activity, diabetes, obesity, and smoking, living with chronic conditions, such as cardiovascular, respiratory, metabolic, and mental health issues, also raises the risk of AFib.
Research from recent studies sheds light on lifestyle choices, comorbidities, and socio-economic factors that might impact AFib occurrence and severity. Participating in a multidimensional, personalized care approach helps manage AFib and reduce complications and mortality.
Dr. Stephen Tang, a cardiac electrophysiologist, broke it down for Medical News Today:
"Managing AFib goes beyond just prescribing oral anticoagulation for stroke prevention or using medication for rate or rhythm control. This condition is complex with numerous contributing factors."
"Identifying and managing these contributing factors is crucial for long-term AFib control," added Dr. Tang.
Risk factors and treatments for AFib
AFib is a condition where the left upper chamber of the heart beats irregularly, which can result in blood clots inside the atrium. If these clots move to the brain, they can block blood flow and result in a stroke. Notably, AFib is a significant risk factor for stroke.
Some non-modifiable risk factors for AFib include genetics, sex, and age. However, other risk factors like lifestyle factors, comorbidities, and socio-economic factors are modifiable.
Lifestyle changes, medications, and in some cases, invasive procedures can help manage this condition. Blood thinners, or anticoagulants, can reduce the risk of blood clot formation and, subsequently, stroke.
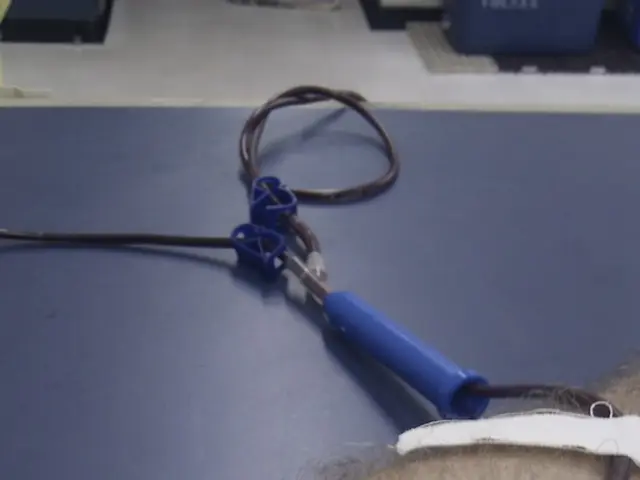
Traditional oral anticoagulants, like warfarin, were commonly prescribed, but new nonvitamin K antagonist oral anticoagulants (NOACs) have become the popular first line of treatment for AFib. Other drugs, like beta-blockers and calcium channel blockers, are also used to control heart rate. In cases where these methods aren't effective, invasive procedures like catheter ablation may be necessary to restore a normal heart rhythm.
Lifestyle factors influencing AFib risk
As with other heart issues, lifestyle factors like physical activity levels, obesity, smoking, and alcohol consumption impact AFib risk.
Physical Activity
Regular physical activity is linked to a lower AFib risk, while a sedentary lifestyle increases the chance of AFib. Individuals who perform at least 150 minutes of moderate-to-vigorous exercise each week are less likely to develop AFib.
Obesity
Obesity is a risk factor for AFib and can make it more likely to recur, complicate catheter ablation, result in stroke, and increase mortality. Weight loss can reduce the risk of AFib recurrence and complications.
Smoking and alcohol consumption
Smoking and heavy alcohol consumption are associated with an increased AFib risk, with evidence suggesting a dose-dependent relationship. The impact of moderate-to-low alcohol consumption is less clear.
Health conditions co-occurring with AFib
In addition to being risk factors for AFib, various chronic conditions may increase the chances of AFib complications.
Obstructive sleep apnea
Obstructive sleep apnea, a condition characterized by airway blockage during sleep, affects around 21-74% of individuals with AFib. This can accelerate blood clot formation, change the heart's structure, and raise the risk of AFib recurrence after catheter ablation. Using a continuous positive airway pressure (CPAP) machine to manage sleep apnea reduces the risk of AFib.
Cardiovascular conditions
Conditions like coronary artery disease, hypertension, heart failure, and cardiomyopathies are more common in individuals with AFib and can raise complications, like stroke or heart failure, and mortality rates. Managing and treating these comorbid cardiovascular conditions can help reduce AFib recurrence or complications.
Metabolic conditions
While diabetes raises the risk of AFib, the relationship between high cholesterol levels and low-density lipoprotein (LDL) levels and AFib is less clear, with some studies indicating a lower risk of AFib. However, higher levels of triglycerides are associated with an increased risk of AFib.
Kidney function
Half of all individuals diagnosed with AFib show impaired kidney function, which can interfere with medication metabolism, raise the risk of adverse effects, and increase complications during catheter ablation.
Respiratory conditions
Chronic obstructive pulmonary disease (COPD) links to a twofold higher risk of AFib. Some COPD medications can trigger faster heart rhythms, but others do not negatively affect individuals with AFib. Short-term exposure to air pollution has also been linked to an increased risk of AFib.
Mental health
Studies have shown that stress and depression are associated with an increased risk of AFib. Mental health conditions may impact adherence to medications, potentially leading to drug interactions. While there's a lack of evidence to connect cognitive impairment and dementia to AFib, dementia negatively influences outcomes in those with AFib.
Impact of comorbid conditions and multiple medication use
Individuals with AFib are more likely to have other chronic conditions, which can raise the risk of complications involving stroke and mortality. The presence of these coexisting chronic conditions requires the use of multiple medications, increasing the risk of adverse effects.
Polypharmacy, or the use of five or more drugs, is associated with an increased risk of complications in individuals with AFib. As a result, managing comorbidities and their medications effectively is essential.
Other risk factors for AFib
Sex, socio-economic status, and ethnicity can also influence the risk of AFib. Some research suggests that people of South Asian and African origin have a lower risk of AFib than white people, which contradicts the higher risk of other heart issues in South Asian people. Studies in the United States reported that white individuals have a higher risk of AFib. In terms of biological sex, men are more likely to develop AFib, but women face a higher risk of complications like stroke and mortality. Women might be undertreated with anticoagulants because of a lack of social support and access to healthcare required to monitor the warfarin dose. Low socioeconomic status is associated with a higher risk of heart failure, stroke, and mortality in those with existing AFib. Access to healthcare may impact the management of risk factors effectively, while a lower health literacy rate may affect patient participation in treatment decisions.
Need for individualized care for AFib
Given the role of multiple factors, including lifestyle choices, comorbidities, genetics, and socio-economic factors, personalized care is necessary. Dr. Nikhil Warrier, a cardiac electrophysiologist, emphasized the need for individualized care:
"Different patients may have different underlying risk factors that increase the likelihood of poor AFib-related outcomes. For example, a patient with a primary AFib trigger of alcohol might need a conversation about alcohol reduction, while a sedentary patient might need a conversation about starting an exercise program."
"Treatment strategies for AFib differ based on the persistence of the arrhythmia, along with age and other modifiable risk factors of the patient. Some patients may respond better to ablation as a first treatment option, while others may not," added Dr. Warrier.
Dr. Yehoshua Levine, a cardiologist, noted: “Optimal management of AFib is very patient-dependent and involves consideration of multiple clinical, socioeconomic, and demographic factors, which are all important in determining the most appropriate treatment approach."
In conclusion, understanding the various factors that contribute to AFib is essential for managing and reducing the risk of complications. Given the complexity of this condition, personalized treatment tailored to the individual is necessary for optimal management and outcomes.
- Research reveals that living with chronic conditions such as cardiovascular, respiratory, metabolic, and mental health issues increases the risk of Atrial Fibrillation (AFib).
- Dr. Stephen Tang, a cardiac electrophysiologist, explains that managing AFib requires more than just prescribing oral anticoagulation for stroke prevention or using medication for rate or rhythm control.
- Some non-modifiable risk factors for AFib include genetics, sex, and age, but other risk factors like lifestyle factors, comorbidities, and socio-economic factors are modifiable.
- Lifestyle changes, medications, and in some cases, invasive procedures can help manage AFib, with blood thinners, or anticoagulants, reducing the risk of blood clot formation and subsequent stroke.
- Obesity is a risk factor for AFib and can increase the chance of recurrence, complicate catheter ablation, result in stroke, and increase mortality. Weight loss can help reduce this risk.
- Obstructive sleep apnea affects around 21-74% of individuals with AFib and can accelerate blood clot formation, change the heart's structure, and raise the risk of AFib recurrence after catheter ablation.
- Chronic kidney disease is common among individuals diagnosed with AFib, interfering with medication metabolism, raising the risk of adverse effects, and increasing complications during catheter ablation.
- Mental health conditions like stress and depression are associated with an increased risk of AFib and may impact adherence to medications, potentially leading to drug interactions.