Personalized Care Focusing on Lifestyle Factors Might Decrease AFib Risk
Atrial fibrillation, commonly known as "AFib," is a prevalent heart condition marked by an irregular heartbeat. Beyond well-established heart health factors like exercise, obesity, and smoking, AFib risk is also associated with chronic conditions, such as metabolic, cardiovascular, respiratory, and mental health issues.
A recent review consolidated data from prior studies on lifestyle choices, comorbidities, and socioeconomic factors that may shape AFib risk. Emphasizing the necessity for comprehensive, personalized care to tackle AFib and minimize death and complication risks, the review called for a multidisciplinary approach to treatment.
Dr. Stephen Tang, a cardiac electrophysiologist, succinctly summarized: "This complex disease isn't just about oral anticoagulation for stroke prevention or controlling the heart rate through medication or ablation. Managing atrial fibrillation requires tackling numerous risk factors and comorbidities."
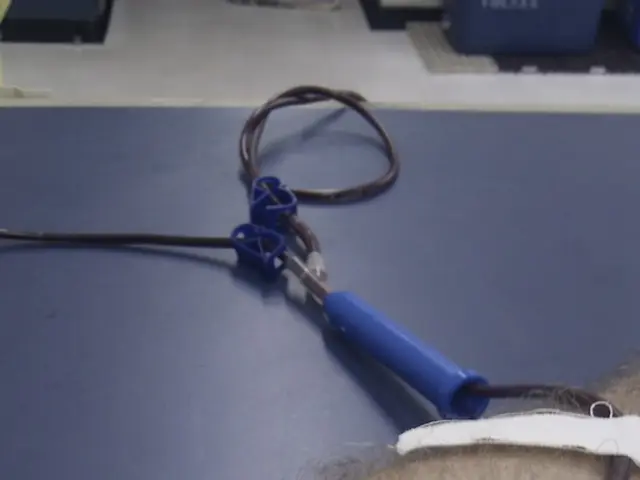
Genetic factors, sex, and age are non-modifiable AFib risk factors. Addressable factors include lifestyle modifications and medication for managing this cardiovascular condition. Blood thinners, or anticoagulants, help reduce the risk of blood clot formation and stroke. Nonvitamin K antagonist oral anticoagulants (NOACs) have surpassed traditional vitamin K drugs as first-line atrial fibrillation treatment.
Regarding lifestyle factors, regular exercise and high-intensity interval training can lower AFib risk and improve overall well-being. Maintaining a healthy weight reduces the risk of AFib recurrence and complications. Additionally, limiting smoking and moderating alcohol consumption can help curtail AFib instances.
Obstructive sleep apnea, a breathing disorder common in individuals with AFib, can raise the risk of blood clots and heart structural changes. Using a continuous positive airway pressure (CPAP) machine for sleep apnea management can help reduce AFib onset, recurrence, and progression.
Individuals with pre-existing cardiovascular conditions like hypertension, heart failure, and coronary artery disease face an increased AFib risk. The management and treatment of coexisting cardiovascular conditions can help reduce AFib recurrence or complications, such as stroke.
Diabetes is associated with a heightened AFib risk, but evidence on sugar control's impact on AFib is mixed. High cholesterol levels, generally linked to cardiovascular diseases, are associated with a lower AFib risk, whereas higher triglyceride levels are linked to increased AFib risk.
Chronic kidney disease can complicate anticoagulant drug metabolism, and individuals with AFib and kidney disease experience more catheter ablation complications. Short-term exposure to air pollution increases AFib risk, though evidence on long-term exposure is limited.
Chronic obstructive pulmonary disease (COPD) and mental health conditions, such as stress and depression, are linked to a higher AFib risk. The precise mechanisms are unclear but may impact medication adherence or drug interactions.
Polypharmacy, i.e., using five or more medications, is associated with an increased risk of complications in individuals with AFib. Carefully balancing the benefits and risks is crucial when considering anticoagulant therapy for at-risk patients.
Differences in lifestyle choices, socioeconomic status, and ethnicity/race influence the risk of AFib. South Asian and African populations may face a lower AFib risk than white people, while females are more likely to develop complications, including stroke and death. Access to healthcare and social support could contribute to disparities in atrial fibrillation management.
The need for tailored, multidisciplinary care is clear, with treatment strategies depending on individual factors. Dr. Nikhil Warrier, a cardiac electrophysiologist, noted that "Underlying risk factors for AFib might differ for each patient, requiring customized conversations about lifestyle modifications and appropriate treatment options."
In conclusion, understanding the various lifestyle factors, comorbid conditions, and socioeconomic implications is key to managing AFib effectively and improving cardiovascular health. By prioritizing lifestyle modification, managing comorbidities, and adopting a personalized treatment approach, individuals can reduce their risk of developing AFib and improve their prognosis.
Lifestyle Factors: Regular exercise, maintaining a healthy weight, limiting smoking, moderating alcohol consumption, ensuring good sleep qualityComorbid Conditions: Hypertension, diabetes mellitus, obstructive sleep apnea, heart conditions, thyroid disease, chronic lung disease.
- Science has revealed that regular exercise and high-intensity interval training can lower the risk of Atrial Fibrillation (AFib) and improve overall well-being.
- Maintaining a healthy weight can reduce the risk of AFib recurrence and complications.
- Limit smoking and moderating alcohol consumption can help curtail AFib instances.
- Obstructive sleep apnea, a common comorbid condition in individuals with AFib, can raise the risk of blood clots and heart structural changes.
- Polypharmacy, using five or more medications, is associated with an increased risk of complications in individuals with AFib.
- Chronic lung disease, such as Chronic Obstructive Pulmonary Disease (COPD), is linked to a higher AFib risk.
- Mental health conditions, including stress and depression, are associated with a higher AFib risk.
- Evidence on sugar control's impact on AFib is mixed, but diabetes is associated with a heightened AFib risk.
- The management and treatment of coexisting cardiovascular conditions like hypertension, heart failure, and coronary artery disease can help reduce AFib recurrence or complications.
- Genetic factors, sex, and age are non-modifiable AFib risk factors, while lifestyle modifications and medication can help manage this cardiovascular condition.